Pediatric Speech Therapy FAQs
What is speech-language pathology?
Speech-language pathology is a health profession aimed at helping individuals develop effective communication and swallowing skills. Professionals in this field are educated and trained to evaluate and treat children and adults with speech, language and swallowing problems.
What are the credentials next to your name? What do they mean?
Many speech therapists have the credentials “CCC-SLP” after their names. This means that the therapist has been awarded their Certificate of Clinical Competence in Speech Language Pathology by ASHA.
What is addressed in your speech therapy evaluation?
A speech-language evaluation at Metro Therapy Center is performed by a speech-language pathologist to gain insight into a child’s developing speech, language, communication, feeding, and oral function skills. A speech-language pathologist will obtain a variety of scores from the tests utilized in the evaluation. These scores (standard scores, age equivalents and percentile ranks), as well as information from other types of tests, help the speech-language pathologist determine if a child has delayed or disordered language. In addition to determining if a language delay or disorder is present, speech-language pathologists at Metro Therapy Center may give informal/formal assessments, observational scales and parent report measures to gather information about social, play, communicative, feeding and behavioral patterns. A report is generated that uses this information to help other professionals make diagnostic decisions and to make recommendations for intervention.
My daughter did not qualify for speech therapy in her public school. Does that mean that she will outgrow her speech problems? Will she qualify for outpatient services?
The state has specific requirements that children must meet to receive speech or language therapy in school. Additionally, the disability must have a negative impact on the student’s education. For example, a student who has a lisp that does not affect her ability to spell or discourage her from participating in class may not qualify for services in the school. However, insurance may cover these services in our outpatient setting.
I want to get extra speech therapy for my child this summer. He gets speech once per week at school. What are the benefits to private therapy? Would additional therapy be confusing for my child?
Many of our patients receive services in school and the outpatient setting! The two professionals may collaborate throughout the year, discussing the student’s goals and progress. Parents must give their consent before professionals can speak about a student. Private speech-language pathologists usually work with students individually, and can focus on all areas of need.
How long does speech therapy take?
This is highly dependent on the individual. Each case needs to be looked at individually and discussed with the professionals, family members, and patients involved.
At what age should I seek out help for my child?
Our speech-language pathologists work with children from infancy to adolescence. If you are concerned about your child’s communication skills, please call to find out if your child should be seen for a communication evaluation and/or consultation.
Why is my speech therapist recommending occupational therapy?
A referral to occupational therapy may be recommended if there are concerns regarding safety, social/emotional development, sensory/emotional regulation, and/or delays in developmental milestones. This way, your speech therapist and occupational therapist can work as a team to develop a treatment plan that is best for your family.
At Metro Therapy Center, we believe in providing holistic, comprehensive care. As part of our intake forms, we include information relating to occupational therapy. If your case history indicates that you would benefit from an occupational therapist, a referral will be placed for a screening or evaluation. In order to maximize the benefit of therapeutic services, including an occupational therapist will be considered the gold standard of care for your child. You can postpone the recommendations; however, we will revisit our plan of care in three months to see how therapy has progressed without the support of all recommended team members. At that time, we may require the addition of an occupational therapist to your team to ensure best practice.
How does sensory and emotional regulation support speech therapy?
Our practice firmly believes in “regulation before expectation,” and if your child is demonstrating challenges regulating with their external environment, it may be challenging for them to organize their body and access higher level speech, language, and feeding skills. In addition to the skilled individualized therapy they provide, OT supports ST by supporting foundational neurological safety, creating an optimal learning environment for additional ST services.
What are typical speech, language, and hearing milestones for young children (1-2 years old)?
Hearing & Understanding Milestones
- Child points to a few body parts when prompted.
- Child follows simple commands and understands simple questions (e.g., “Roll the ball,” “Kiss the baby,” “Where’s your shoe?”).
- Child listens to simple stories, songs, and rhymes.
- Child points pictures in a book when they’re mentioned.
http://www.asha.org/public/speech/development/12.htm
Talking Milestones
- Child’s vocabulary grows every month.
- Child begins using some one- or two- word questions (e.g., “Where kitty?”, “Go bye-bye?”, “What’s that?”).
- Child puts two words together (e.g., “More cookie,” “No juice,” “Mommy book”.)
- Child uses many different consonant sounds at the beginning of words.
- For a complete guide to children’s milestones, visit:
What can I do to help improve my child’s speech and language development?
- Model language from your child’s perspective! When adults talk with children, they provide a model for children to emulate. Kids can learn about language, intonation and speech patterns when they listen to adults’ voices
- Narrate family daily routines to stimulate their children’s speech and language development. Such occasions include, but are not limited to feeding, dressing, playtime, and bath-time.
My child has chronic ear infections. Recently, another parent warned me that ear infections can be very problematic for speech and language development. Should I be concerned about my child’s recurring ear infections?
When children have ear infections (otitis media), fluid can build up in their middle ear. When this occurs, it can affect how they hear sounds. The sounds that they hear may seem distorted. For instance, imagine what it would sound like to hear someone talking while your head was under water. In order to learn to speak, children need to be able to hear speech sounds accurately and clearly. If they experience frequent ear infections while their language is developing, they may be at risk for speech and language problems.
How do I know if my child is Autistic?
What we’ve traditionally thought about regarding Autism is constantly evolving. Autism is a spectrum for a reason. If we’ve met one Autistic child, we’ve met one Autistic child! For more information on Autism and neurodivergence, please see this link: https://my.clevelandclinic.org/health/symptoms/23154-neurodivergent. Your therapist is more than willing to discuss this in-depth with you regarding your individual child.
What is the difference between ‘expressive’ and ‘receptive’ language?
In general, speech therapists aim to improve both their client’s “Expressive” and “Receptive” language skills. Receptive language refers to the ability to understand spoken language and follow directions. For example, a child’s ability to listen to and follow the directions, “point to your shoe,” relies on their receptive language. Typically, children are able to understand language prior to being able to produce it, themselves. A child who is unable to comprehend language may have receptive language difficulties. In contrast, expressive language refers to the ability to communicate verbally or with written words. Children that have difficulty communicating their wants and needs may have expressive language difficulties. For example, children might be experiencing expressive language difficulties if they are unable to inform their caregivers that they are hungry. It is important to note that this is just one example of an expressive language difficulty. If you have concerns about your child’s speech and/or language development, you should consult with a pediatric speech-language pathologist.
Pediatric speech-language pathologists work with children exhibiting either or both receptive and expressive language difficulties. Receptive and expressive language can be improved by providing language stimulation. Parents of young children (ages 1-3) can improve their children’s receptive and expressive language by repeating what their children says, and expanding on those utterances. If the child says, “Ball,” the parent can then expand on that utterance by saying something like, “Yes, you have a big ball.” The child will then begin to learn from their caregiver’s model, and should gradually begin to combine multiple words together to form phrases.
What is analytical language processing? What is gestalt language processing?
What are motor speech disorders?
- Dysarthria: This is when the muscles of the mouth, face, and respiratory system may become weak, move slowly, or not move at all. Sometimes people refer to dysarthric speech as “slurred” speech.
- Apraxia: The term apraxia (dyspraxia) is used to describe a child who is exhibiting difficulty with praxis (performing an action). Childhood Apraxia of Speech is a label/category of a speech sound disorder that is explained by difficulties with planning and/or programming of the motor movements that result in speech. Our speech-language pathologists have received training in Dynamic Temporal and Tactile Cueing (DTTC) for Childhood Apraxia of Speech. People with apraxia of speech have trouble sequencing the sounds in syllables and words.
What is stuttering?
- Repetitions: Part-word ( e.g., “dddd dog”), whole-word ( e.g., “How How How How; are you”?), phrase (e.g., “My name is.. My name is .. My name is…Bob.”)
- Prolongations: Silent prolongations known as “blocks”.
- Sound prolongations ( e.g., “sssssomebody”.)
- Interjections: Sound /syllable ( e.g., “I go to um.. um .. um high school.”)
- Word (e.g., “I want uh like like like go home.”)
- Phrase (e.g., “This is um like um like um like my friend.”)
- Pauses
- Broken Words
- Incomplete Sentences
- Revisions
What is an auditory processing disorder?
Listening is an active process of hearing and comprehending what is said. Auditory processing is what we do with what we hear. An auditory processing disorder (APD) is a difficulty in processing auditory information although hearing and intellectual ability are unimpaired. Areas that may be affected by an auditory processing disorder are:
- Receptive language and vocabulary
- Auditory memory for meaningful and non-meaningful information of increasing length and complexity: Meaningful information involves the ability to recall directions and interpret them. Non-meaningful information is the ability to recall unrelated words and numbers.
- Phonological awareness skills: That is, an individual’s explicit knowledge of the sound segments (phonemes) which form words. These skills consist of being able to blend, delete, substitute, rhyme, segment and isolate sounds. Difficulties in the area of phonological skills may precede difficulties in reading and spelling.
- Thinking and reasoning: the ability to use common sense and ingenuity to solve common thought problems.
- Auditory vigilance: the awareness of and response to sound. For example, knowing that your name was called and giving a response to the fact that your name was called.
- Auditory discrimination: the ability to discriminate paired words with phonemically similar consonants, cognates and vowel differences.
Will raising children in a bilingual home affect their language development?
What is Aphasia?
Listening is an active process of hearing and comprehending what is said. Auditory processing is what we do with what we hear. An auditory processing disorder (APD) is a difficulty in processing auditory information although hearing and intellectual ability are unimpaired. Areas that may be affected by an auditory processing disorder are:
- Receptive language and vocabulary
- Auditory memory for meaningful and non-meaningful information of increasing length and complexity: Meaningful information involves the ability to recall directions and interpret them. Non-meaningful information is the ability to recall unrelated words and numbers.
- Phonological awareness skills: That is, an individual’s explicit knowledge of the sound segments (phonemes) which form words. These skills consist of being able to blend, delete, substitute, rhyme, segment and isolate sounds. Difficulties in the area of phonological skills may precede difficulties in reading and spelling.
- Thinking and reasoning: the ability to use common sense and ingenuity to solve common thought problems.
- Auditory vigilance: the awareness of and response to sound. For example, knowing that your name was called and giving a response to the fact that your name was called.
- Auditory discrimination: the ability to discriminate paired words with phonemically similar consonants, cognates and vowel differences.
What is Dysarthria?
Aphasia is a language disorder, usually caused by damage to the left side of the brain. There are different types of aphasia that affect people in various ways. Aphasia can make it difficult for a person to understand spoken or written information. It can also affect a person’s ability to speak or write. Sometimes an individual can have impairments in all of these areas to some degree. The different types of aphasia are known as global, Broca’s, transcortical motor, conduction, anomic, transcortical sensory and Wernicke’s aphasia.
What is a voice disorder?
Voice is the sound produced by vibration of the vocal cords (vocal folds) in the larynx (voice box). A voice disorder occurs when the vocal folds do not vibrate effectively to produce a clear sound.
Common Causes:
Causes of voice disorders can include abuse or misuse of the voice, such as yelling, excessive throat clearing, or speaking too loudly. These types of behaviors result in excessive hard closure of the vocal folds causing blister-like bruises that can harden into callous-like lesions called vocal fold nodules. Other causes of voice disorders can include Laryngo-Pharyngeal Reflux (excessive stomach acid backing into the larynx), vocal fold polyps, vocal fold paralysis, vocal fold cysts, etc.
Symptoms of Voice Disorders:
- Voice quality disturbance: breathiness, raspiness, harshness
- Voice pitch disturbance: pitch too high for age and gender, pitch too low for age and gender, pitch fluctuates excessively, pitch is monotone
- Voice volume is too low or too loud
- Vocal fatigue (decreased stamina, increased hoarseness following speaking)
- Effortful voice use (having to use too much effort to speak)
Evaluation of Voice Disorders:
Voice evaluations are conducted by Speech-language pathologists who are experts in the area of voice. Evaluations include non-instrumental assessment and instrumental assessment. These assessments allow the Speech-language pathologist to measure the voice objectively, determine patterns that suggest how the larynx is functioning physically, and determine whether there is a hyper functional or hypo functional component present. Voice disorders are complex and this type of evaluation helps determine whether behavioral voice therapy, surgery or a combination of approaches would best serve the patient.
Treatment Options:
Types of voice treatment may include:
- Vocal strengthening- exercises that can improve voice quality and stamina and can also reduce symptoms of vocal effort and fatigue. Examples of exercises are repetitions of high speech sounds, pitch glides, or glottal closure. These exercises are often used with singers.
- Reduction of vocally abusive behaviors- During the evaluation and interview, vocally abusive behaviors are often identified. Some examples include: talking in competition with background noise, yelling, throat clearing, loud cell phone use, not using a microphone, etc. In the treatment session, goals can be made to improve or eliminate these behaviors and provide strategies for care of the voice.
- Improvement in vocal technique- improving respiratory support for proper voice use, reducing hard glottal attack, and improving vocal resonance. Goals are created during voice therapy sessions and home exercises are provided for continued practice. Carryover of these techniques into everyday situations is also expected.
Pre and Post surgical treatment- Counseling of proper voice care before and/or after vocal fold surgery can significantly improve surgical outcomes and assist patients in healthy return to voice use following surgery. Patients can expect gradual return to voice use following surgery.
Will insurance help pay for speech therapy?
Health insurance may sometimes cover speech and language therapy. There are variations in coverage based on carriers, individual’s policy and diagnosis. Be aware of restrictions, deductibles and co-payments. Please contact your insurance carrier for more information about your coverage.
What is the difference between speech therapy and ABA therapy? Do you provide ABA therapy?
Our speech therapists collaborate with all members of your child’s care team, although we do not provide ABA therapy.
ABA (Applied Behavior Analysis) is a behavior-based approach. It focuses on modifying behaviors using reinforcement (rewards or consequences). ABA often breaks tasks into small steps and encourages repetition to build skills through extrinsic motivation.
Often, behaviors happen because a child is trying to communicate something, such as being overwhelmed, needing a break, or wanting something they can’t yet ask for. Our speech therapists do the detective work to determine how your child communicates, what might be making communication challenging, and honoring their unique way of interacting with the world. Our goal is to give your child tools to express themselves in their own way through fostering intrinsic motivation to communicate. Speech therapy at MST is strength-based and individualized, which means your child will learn through play and real-life, naturalistic interactions, rather than rote memorization. The therapist will follow your child’s lead, building trust and encouraging natural communication. Instead of focusing on stopping behaviors (like hand-flapping or meltdowns), our speech therapists, in collaboration with our occupational therapists, try to understand the “why” behind the behavior. This is what neuro-affirming care means to us!
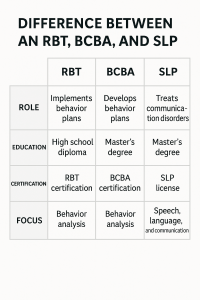
What are the educational difference between a BCBA, RBT, and an SLP?
Both a Board Certified Behavioral Analyst (BCBA) and Speech Language Pathologist (SLP) require a master’s degree, supervised clinical hours, and a board certification exam.
SLPs complete a supervised clinical experience of at least 400 hours during graduate school that must include work with individuals across the lifespan and with various types of severities of communication and/or related disorders (voice, fluency, swallowing, language, speech, articulation, AAC, etc). Following graduation, an SLP must complete a supervised clinical fellowship of more than 1,400 hours.
BCBAs complete supervised independent fieldwork that includes at least 1,500 hours of supervised fieldwork, a practicum of at least 1,000 hours, and an intensive practicum of at least 750 hours. They focus on modifying behaviors using reinforcement (rewards or consequences).
An Registered Behavior Technician (RBT), has at minimum a high school diploma and a 40-hour coursework curriculum. They must be supervised by a BCBA, and have the most contact time with a child. RBT’s cannot create treatment plans, but they can follow a treatment plan created by a BCBA.
Adult Speech Therapy FAQs
What is Adult Speech Therapy?
Adult speech therapy can be used to help manage speech, language, cognitive, eating or swallowing symptoms that result from medical conditions such as a stroke or dementia, or from the onset of motor-skill affecting conditions like Parkinson’s Disease or Multiple Sclerosis. Brain injury and accidents that cause damage to the throat, jaw, or facial structure can also impair speaking ability. Other people may benefit from adult speech therapy due to underlying neurodiversity, which affect comprehension of language or participation in activities of daily living.
Diagnosis of a speech or language disability is done through a variety of tests. Once the specific underlying cause is identified, treatment programs to help the patient can begin.
Treatment done in adult speech therapy may be done in many different ways, as best fits the need of the patient. Therapy is always tailored to the individual to improve overall quality of life. Depending on the nature of the condition, exercises for muscular improvement and homework may also become a part of the program.
What is transgender voice therapy?
Transgender voice therapy is a form of therapy that focuses on helping individuals with gender dysphoria to modify their voice to match their gender identity. This may include training in pitch, resonance, and intonation.
When might an adult need cognitive therapy?
An adult might need cognitive therapy if they have difficulty with attention, memory, perception, or problem-solving due to a physical or mental condition. Examples of conditions that may benefit from cognitive therapy include stroke, brain injury, and dementia.
When might an adult need swallowing therapy?
An adult might need swallowing therapy if they have difficulty swallowing food or liquids due to a physical or neurological condition. Examples of conditions that may benefit from swallowing therapy include stroke, brain injury, Parkinson’s disease, and throat cancer.
When might an adult develop a stutter?
A stutter can develop at any age, but it often begins in childhood. Some adults may develop a stutter later in life due to neurological conditions or traumatic brain injury.
How does stuttering affect communication?
Stuttering can affect communication by making it difficult for individuals to express themselves fluently. It can cause frustration, anxiety, and avoidance of certain speaking situations.
Can stuttering be treated?
At Metro Therapy Center we encourage open stuttering, reducing avoidance behaviors, and increasing self-confidence. Speech and language therapy can help individuals with stuttering to reduce anxiety while communicating and increase confidence in speaking situations.
Can I participate in therapy remotely?
AAC Clinic FAQs
What is AAC, and who can benefit from it?
AAC stands for Augmentative and Alternative Communication. It includes a wide range of tools and strategies that help individuals with communication challenges express themselves effectively. AAC devices can benefit people with various conditions, including but not limited to autism, cerebral palsy, speech disorders, and conditions that affect speech and language abilities.
How do I know if an AAC device is right for me or my loved one?
If you or your loved one is experiencing difficulty with spoken communication, AAC may be considered. An initial assessment by our therapists will help determine if an AAC device is suitable and which specific strategies or devices may be beneficial.
What types of AAC devices are available?
AAC devices vary and can include low-tech options like communication boards, picture exchange systems, and gestures, as well as high-tech options like speech-generating devices (SGDs) and apps on tablets or smartphones. The type of AAC recommended depends on individual needs and preferences.
How can I get started with AAC therapy at your clinic?
To get started, please contact us to schedule an initial assessment. During this assessment, we will evaluate communication abilities and discuss goals. Following the assessment, we will work together to create a personalized AAC therapy plan.
Is AAC therapy only for children, or can adults benefit from it too?
AAC therapy is not limited to children. Adults with communication challenges, whether due to acquired conditions or lifelong disabilities, can benefit significantly from an AAC device. We provide AAC services for individuals of all ages.
How long does AAC therapy typically last?
The duration of AAC therapy varies depending on individual needs and goals. Some clients may benefit from short-term therapy to address specific communication challenges, while others may engage in ongoing therapy for skill development and support.
Do you offer training for family members and caregivers on using AAC devices and strategies?
Yes, we provide training and support for family members and caregivers to ensure that they are well-equipped to assist with AAC device use and facilitate effective communication with their loved ones.
Are AAC devices covered by insurance or funding sources?
Coverage for AAC devices varies by insurance plans and funding sources. Our team can assist you in navigating insurance claims and identifying potential funding options to help make AAC devices more accessible.
Can AAC therapy improve speech and language skills?
While AAC therapy primarily focuses on alternative communication methods, it can also complement speech and language development. Our therapists work to enhance overall communication skills, which include speech.
How can I schedule an appointment or learn more about your AAC services?
To schedule an appointment or inquire about our AAC services, please contact our clinic by phone or email. Our team is here to assist you and provide the information you need.
Contact Us for More Information
If you have additional questions or need further clarification, please don’t hesitate to reach out to us. We are committed to providing you with the information and support you need to make informed decisions.